Contact Us
Other Articles
2. What is Chemotherapy?
3. What is Radiotherapy?
4. Role of Ayurveda in Cancer Treatment
5. Genesis of Cancer
6. Early Detection of Cancer
7. Diet, Nutrition & Cancer
8. Tobacco Smoking & Cancer
9. Conventional Treatment of Cancer
10. Soft Tissue Sarcoma
11. Mesothelioma
12. Skin Cancer
13. Bone Cancer
14. Leukaemia
15. Chronic Lymphocytic Leukaemia (CLL)
16. Chronic Myelogenous Leukaemia (CML)
17. Acute Lymphocytic Leukaemia (ALL) & Acute Non-Lymphocytic Leukaemias (ANLL)
18. Acute Myelogenous Leukaemia (AML)
19. Lymphoma
20. Multiple Myeloma
21. Breast Cancer
22. Prostate Cancer
23. Oral Cancer (Carcinoma of the Cheek, Lips & Tongue)
24. Carcinoma of the Salivary Gland
25. Carcinoma of the Paranasal Sinus
26. Carcinoma of Pharynx (Oropharynx, Nasopharynx and Hypopharynx)
27. Carcinoma of the Larynx
28. Brain & Spinal Cord Tumours
29. Primary Tumours of the Brain
30. Metastases in the Brain
31. Carcinoma of the Oesophagus
32. Thyroid Cancer
33. Bronchogenic Carcinoma (Lung Cancer)
34. Secondary Cancers of the Lung
35. Carcinoma of the Stomach
36. Liver Cancer
37. Gallbladder & Biliary Tract Cancer
38. Pancreatic Cancer
39. Kidney Cancer (Renal Cell Carcinoma and Nephroblastoma)
40. Urinary Tract (Transitional Cell Carcinoma) & Bladder Cancer
41. Carcinoma of Colon & Rectum
42. Primary Tumours of the Testis
43. Ovarian Cancer (Stromal, Germ Cell and Krukenberg's Tumour)
44. Carcinoma of Uterus
45. Cervix Cancer
46. Paediatric Cancers
47. AIDS Related Cancers
48. Carcinoma of Unknown Primary Site (CUPS)
49. Role of Nutrition in Cancer Treatment
50. Chinese Medicine in Cancer Treatment
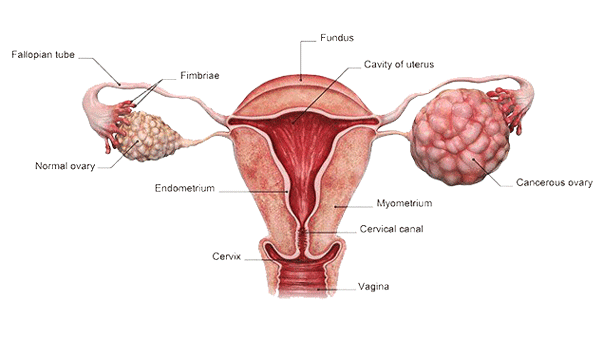
Carcinoma of the ovary is one of the leading causes of death in women. It
usually affects the elderly women during 60 to 80 years of age. Carcinoma of
the ovary has a higher incidence in industrialised nations. The exact cause is
not fully understood, but it appears that hormones play an important role in
genesis of the ovarian carcinoma. Studies have shown that the risk of ovarian
carcinoma is reduced to 50 per cent during pregnancy due to hormonal factors.
The use of contraceptive pills also lowers the risk of ovarian carcinoma
because it creates a hormonal balance in the body that is similar to the
pregnancy. Studies have revealed that the nulliparous women are more likely to
develop the ovarian carcinoma. Those women, who had suffered from cancer of the
breast, intestine or the rectum, also have a higher risk of the ovarian
carcinoma. It has been observed that those women, who had a positive family
history of the breast or the ovarian cancer, have a higher risk of the ovarian
carcinoma. Exposure to radiation and asbestos are the other risk factors. About
85 per cent of the ovarian tumours are carcinomas, which include mucinous
cystadenocarcinoma, serous cystadenocarcinoma, clear cell cystadenocarcinoma,
endometrioid adenocarcinoma and undifferentiated carcinoma. The remaining 15
per cent of the ovarian tumours are germ cell tumours, stromal tumours and the
borderline tumours.
Carcinoma of the ovary usually remains asymptomatic during initial stages of the disease. As the disease advances, non-specific gastrointestinal symptoms appear, which include nausea, vomiting, diarrhoea and constipation. The major symptoms of ovarian carcinoma include palpable abdominal mass, ascites and weight loss. In advanced stages, there may be pelvic pressure, vaginal bleeding and abdominal pain or distension. Carcinoma of the ovary usually spreads to peritoneum, omentum and the pouch of Douglas.
Staging of carcinoma of the ovary is done as follows:
- In stage I of the ovarian carcinoma, the tumour is localised in one or both of the ovaries.
- In stage II, the tumour spreads to the uterus, fallopian tubes and other tissues within the pelvis.
- In stage III, the tumour metastasises to the abdominal lymph nodes and abdominal organs such as the intestines and surface of the liver.
- In stage IV, the ovarian carcinoma metastasises to the liver and extra abdominal organs.
- Recurrent ovarian carcinoma is the one that reappears after an apparent recovery in response to the initial treatment.
Procedures used in diagnosis and
evaluation of the ovarian carcinoma include pelvic examination, X-rays,
ultrasound, CT scan, IVP, exploratory laparotomy and biopsy. The estimation of
CA 125 and CEA is important in the follow-up of ovarian carcinoma patients. The
raised level of CA 125 indicates presence of the ovarian carcinoma in the body,
whereas the raised level of CEA indicates advanced stage of the ovarian
carcinoma.
Stromal & Germ Cell Tumours
Ovarian germ cell tumours and stromal tumours constitute about 10 per
cent of the ovarian tumours. Germ cell ovarian tumour arises from the germ
cells (the cells that give rise to ovaries during the foetal development). The
germ cell tumours include dysgerminoma, endodermal sinus tumour, embryonal
carcinoma, malignant teratoma and choriocarcinoma. The stromal tumours include
granulosa cell tumour and Sertoli-Leydig tumour. Ovarian germ cell tumours and
stromal tumours affect young women usually below 20 years of age.
Ovarian germ cell tumours and stromal tumours remain asymptomatic during initial stages of the disease. Common presenting symptoms of the ovarian germ cell tumours and stromal tumours include mass in the abdomen and vaginal bleeding.
Staging of ovarian germ cell tumours and stromal tumours are done as follows:
- In stage I, a germ cell ovarian tumour is localised to one or both ovaries.
- In stage II, the tumour spreads to the uterus, fallopian tubes and other tissues within the pelvis.
- In stage III, a germ cell ovarian tumour metastasises to the abdominal lymph nodes and abdominal organs such as the intestines and surface of the liver.
- In stage IV, the tumour metastasises to the liver and extra abdominal organs.
- Recurrent germ cell ovarian tumour is the one that reappears after an apparent recovery in response to the initial treatment.
Procedures used in the diagnosis and evaluation of a germ cell ovarian tumour include pelvic examination, ultrasound, CT scan and biopsy.
Krukenberg's Tumour
Krukenberg's tumour is a secondary ovarian tumour that has been
metastasised usually from a primary carcinoma of the stomach, large intestine
or the breast. The Krukenberg's tumour has a smooth surface, does not form
adhesions and moves freely in the pelvis. Krukenberg's tumour usually affects
both the ovaries.
Disclaimer:
This content is for information and educational purposes only and should not be perceived as medical advice. Please consult a certified medical or healthcare professional before making any decision regarding your health using the content above.
Click here to go back to the list of all Articles



Ovarian Cancer (Stromal, Germ Cell and Krukenberg's Tumour)